By Dr Mark Ready
History
35 year old female presents with headaches and possible seizure.
Imaging
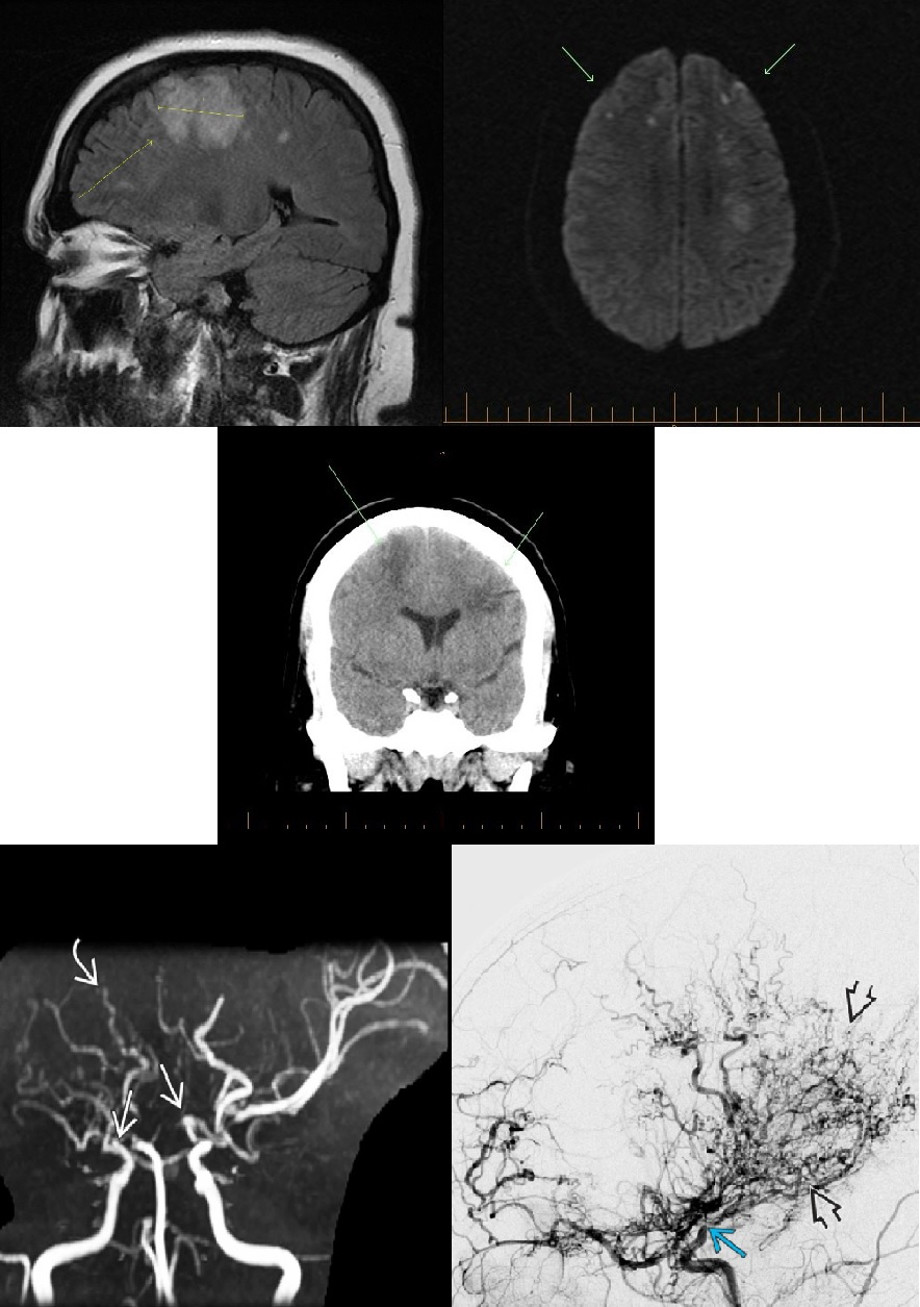
MRI – Bilateral frontal lobe white matter hyperintensity. Diffusion imaging shows areas of restricted diffusion reflecting acute ischemia. Also areas of parechymal and leptomeningeal enhancement bilaterally. Areas of gliosis and left periventricular white matter reflects prior ischemia/infarction.
CT – Areas of reduced density in frontal lobe white matter bilaterally. Extension to involve grey matter more superiorly. No acute hemorrhage.
Summary
Differential diagnosis for these findings.
- Vasculitis.
- Neuro sarcoidosis.
- Encephalitis.
- Septic emboli.
Final diagnosis
MoyaMoya disease.
Discussion
A progressive occlusive arteritis which affects distal ICA vessels into anterior two thirds of the Circle of Willis. Affects children and young adults.
More common in East Asian population.
Primary Moyamoya disease – more common in Japan/Korea.
Secondary – Moyamoya – Acquired.
- Cranial radiation.
- Atherosclerosis.
- Neurofibromatosis.
Usually presents with headaches and recurrent hemi paretic attacks.
Angiography reveals bilateral stenosis/occlusion supraclinoid portion of ICA vessels into anterior cerebral and middle cerebral arteries.
Puff of smoke (Moyamoya in Japanese) appearance in basal ganglia.